Johns Hopkins APL Technical Digest
Wearables-Based Disease Surveillance: SIGMA+ Human Sentinel Networks Concept of Operations

Ivan Stanish, Jane E. Valentine, Damon C. Duquaine, Robert A. Stoll, Ray H. Mariner, and Dorsey R. Woodson
Abstract
The Defense Advanced Research Projects Agency SIGMA+ program developed a persistent, real-time, early warning and detection system for the full spectrum of chemical, biological, radiological, nuclear, and explosive weapon of mass destruction threats at the city to region scale. In support of this program, and leveraging technical expertise in modeling and simulation, applied mathematics, and epidemiology, the Johns Hopkins University Applied Physics Laboratory (APL) characterized and quantified the impact a wearables-based human sentinel network would have on the ability to provide advanced detection of a naturally occurring or intentional biothreat event. Modeling results demonstrate that instrumenting as few as 5% of the population could advance detection of seasonal influenza by 5–14 days and an anthrax attack by ~1 day as compared with traditional public health surveillance. Early detection and geolocation of individuals exposed to biological threats enables timelier and more effective biothreat countermeasures and mitigation strategies.
Download this article or scroll to continue reading
Program Background and Introduction
The Defense Advanced Research Projects Agency (DARPA) SIGMA+ program developed a persistent, real-time, early warning and detection system for the full spectrum of chemical, biological, radiological, nuclear, and explosive (CBRNE) weapon of mass destruction threats at the city to region scale.1 For biological threats, SIGMA+ developed novel methods of environmental and human-based sensing for improved real-time detection of naturally occurring or human-made biothreat events. Relative to the current state of the art, this effort aimed to provide days-earlier detection and geolocation of biological threats, enabling more effective countermeasures and mitigation strategies. DARPA tasked APL to develop a concept of operations (CONOPS) framework centered on an integrated two-tier, human sentinel network (HSN) to enhance current disease surveillance.
APL leveraged previous computational modeling and analysis, engaged stakeholders via formal tabletop exercises (TTXs) and targeted discussions, and conducted additional research and fact-finding in support of preliminary CONOPS development. This research identified key materiel and nonmateriel considerations and risks related to implementation of the proposed HSN, including additional materiel development needs, regulatory compliance issues, participant recruitment and engagement strategies, and data management topics. APL proposed several operational business models, with varying cost estimates and, in some cases, differing nonmateriel considerations and risks. This work, in conjunction with the technological development described above, indicates that instantiation of an HSN program is feasible and would provide value to the public health community, the emergency response community, and individual participants.
Purpose and Scope
Presented here is a CONOPS framework centered on an integrated two-tier HSN concept to enhance the current state of public health disease surveillance. The HSN concept is composed of wearable physiological monitors (hereafter, “wearable sensors”) (tier 1) distributed among a fraction of the adult population. Algorithms processing an individual’s physiological data would generate alerts in the event of a possible biological exposure; following a tier 1 alert, some individuals would be prompted to seek confirmatory testing for one or more pathogens (tier 2). Both the wearable alerts and test results would be reported in real time to a secure cloud-based platform via a dedicated application. The platform would aggregate the information and disseminate it to public health authorities and critical incident response entities.
The SIGMA+ program demonstrated multiple proofs of concept of system components, including:
- High-accuracy presymptomatic/asymptomatic illness alerting via wearable sensors and alerting algorithms in an influenza-challenge cohort study2
- Communications platforms and information management systems to support collection, storage, distribution, and analysis of HSN data
- User interfaces and visualization platforms both for individual HSN participants and for end users and consumers of population-level or group-level data
These components have been integrated into a pilot wearable network instance with stakeholders from Marion County, Indiana. Key considerations related to implementation of an HSN, such as materiel and nonmateriel factors, regulatory compliance, participant recruitment and engagement, data management, and operational business models, are also presented briefly.
Methodology
The analysis approach of this study consisted of three primary activities to inform HSN concept of employment/CONOPS development.
- Modeling. An agent-based model of seasonal influenza and a custom-built probabilistic model for an intentional anthrax release were developed to assess the potential impact an HSN could have on accelerating the timeline of detecting a public health emergency. Each modeled disease characteristics, public health practices, tier 1 and tier 2 phenomena, and individual dynamics to simulate disease outbreaks and HSN detection in a given population. Results showed that if 5% to 25% of the population were instrumented within the proposed HSN, it could advance detection of seasonal influenza by 5–14 days and anthrax by ~1 day as compared with traditional public health surveillance.
- Scientific partnership. This activity involved collaborative work with several SIGMA+ organizations:
- Sandia National Laboratories: development of an integrated environmental-HSN CONOPS
- RTI International: detection algorithm development and physiological wearable studies
- Two Six Technologies: consultation on data storage and processing at scale
- Massachusetts Institute of Technology Lincoln Laboratory: knowledge sharing on related physiological wearable studies and TTX planning
- End user/stakeholder engagements. In coordination with the partners above, APL conducted TTXs and focus groups to elicit feedback on the utility of an HSN to support decision-making and incident response in the face of a public health emergency. Notional use cases, critical infrastructure and data elements, and gaps in planning and risks to operation were chief topic areas. The group engaged US government parties at the national, state, and local levels.
Proposed HSN CONOPS
System Concept Overview
The US public health surveillance system is a multilayer (local, state, and national), heterogeneous network of private, public, and military entities. Surveillance may be active, passive, or syndromic. Traditional detection of outbreaks and public health emergencies is slowed by delays in diagnostic testing and reporting3,4 and is inadequate at estimating the magnitude of these events.5,6
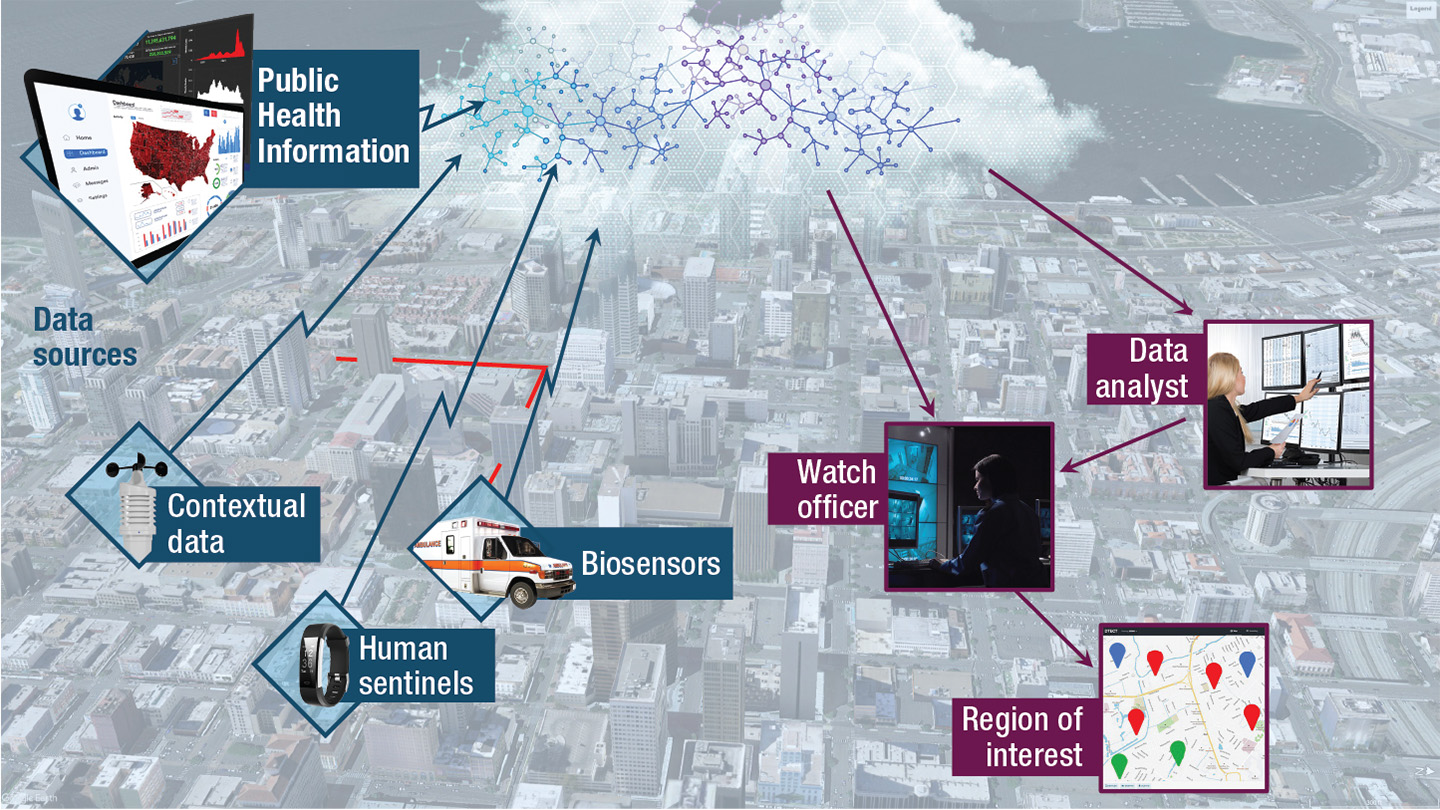
The SIGMA+ program developed a scalable network of sensors and intelligence analytics for the advanced surveillance and detection of CBRNE threats. For biological threats, the proposed system consists of environmental near-real-time aerosol biological sensors monitoring the atmosphere for pathogens (preferably in mobile configurations), an HSN of individuals volunteering to share wearable sensor data (e.g., from smartwatches), and a cloud-based platform that aggregates and analyzes data from the environmental sensors, wearable sensors, and public health sources (Figure 1).
Integrating these novel data sources with existing ones (e.g., syndromic surveillance7) into a single platform will provide an opportunity for improved detection of emerging or crisis public health events through the fusion and analysis of all accessible data, providing comprehensive situational awareness to the public health and law enforcement response.
Figure 1
The envisioned HSN program. Sensor and relevant contextual data are uploaded, aggregated, and analyzed for display and to support decision-making.
HSN Structure and Functionality
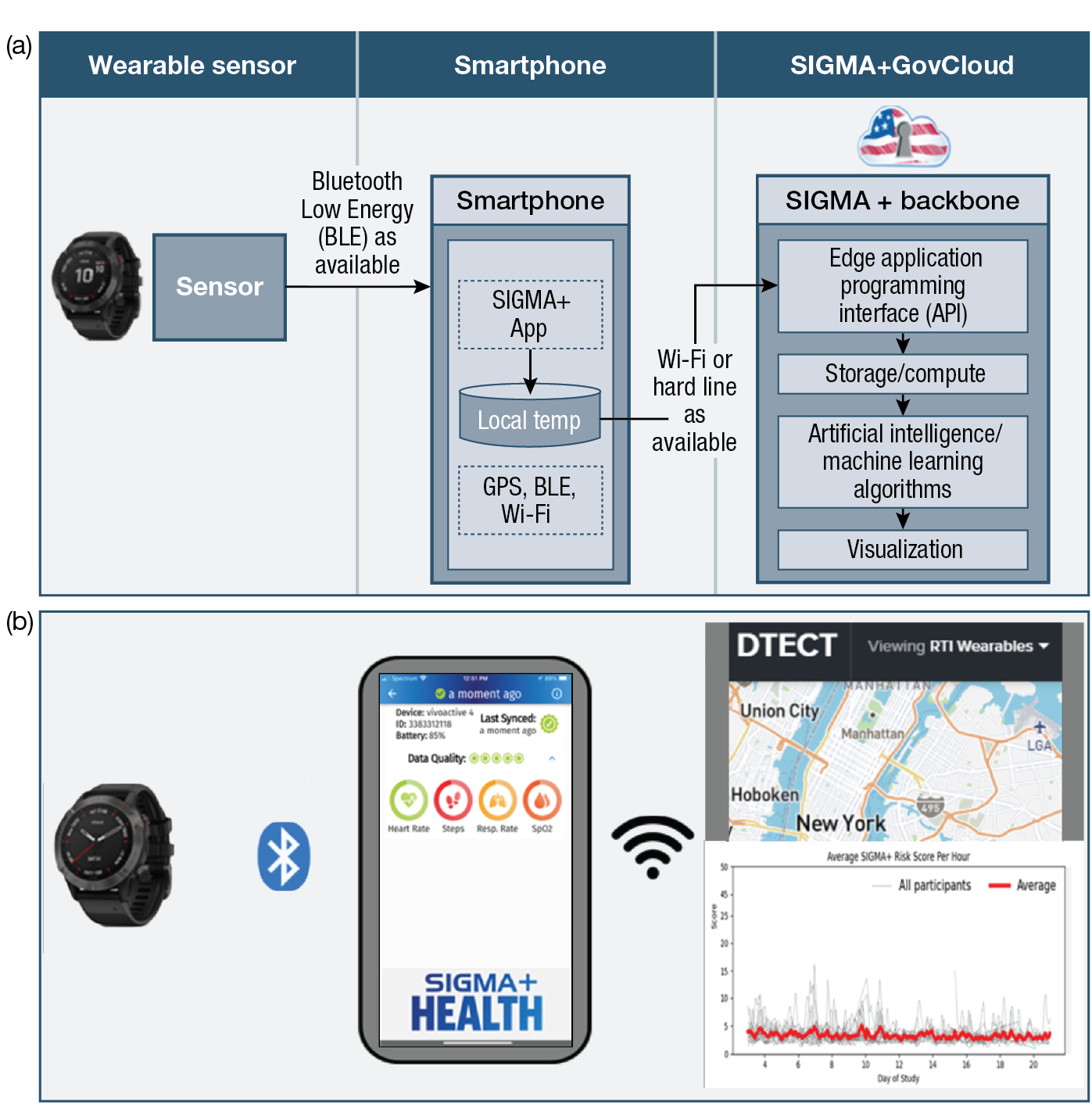
The purpose of the HSN is to significantly improve the speed and fidelity of surveillance of outbreaks and exposures to harmful biological agents. The network would consist of individuals outfitted with wearable sensors (tier 1) to monitor physiological markers, such as heart rate, heart rate variability, peripheral oxygen saturation (SpO2), temperature, sleep quality, and activity levels. Algorithms, currently in the prototype phase, embedded within a smartphone application analyze changes in these markers to detect pre- and asymptomatic illness at the individual level.
HSN Data Flow and Technical Stack
Currently, wearable sensor data are insufficient to establish the cause of an infection. Therefore, deviations from baseline markers would trigger an alert to prompt the wearer to seek diagnostic testing at locations such as sentinel pharmacies or provider offices (tier 2). The alert, along with non-Personally Identifiable Information/Protected Health Information metadata from the wearable device, such as demographics, algorithm parameters triggered, and location, would be sent to the cloud-based platform, integrated with the other public health data streams, and analyzed in near real time (Figure 2 and Figure 3).
Figure 2
HSN data flow. Deviations from baseline markers would trigger an alert to prompt the wearer of the sensor to seek diagnostic testing. The alert, along with metadata from the wearable device, would be sent to the cloud-based platform, integrated with the other public health data streams, and analyzed in near real time.
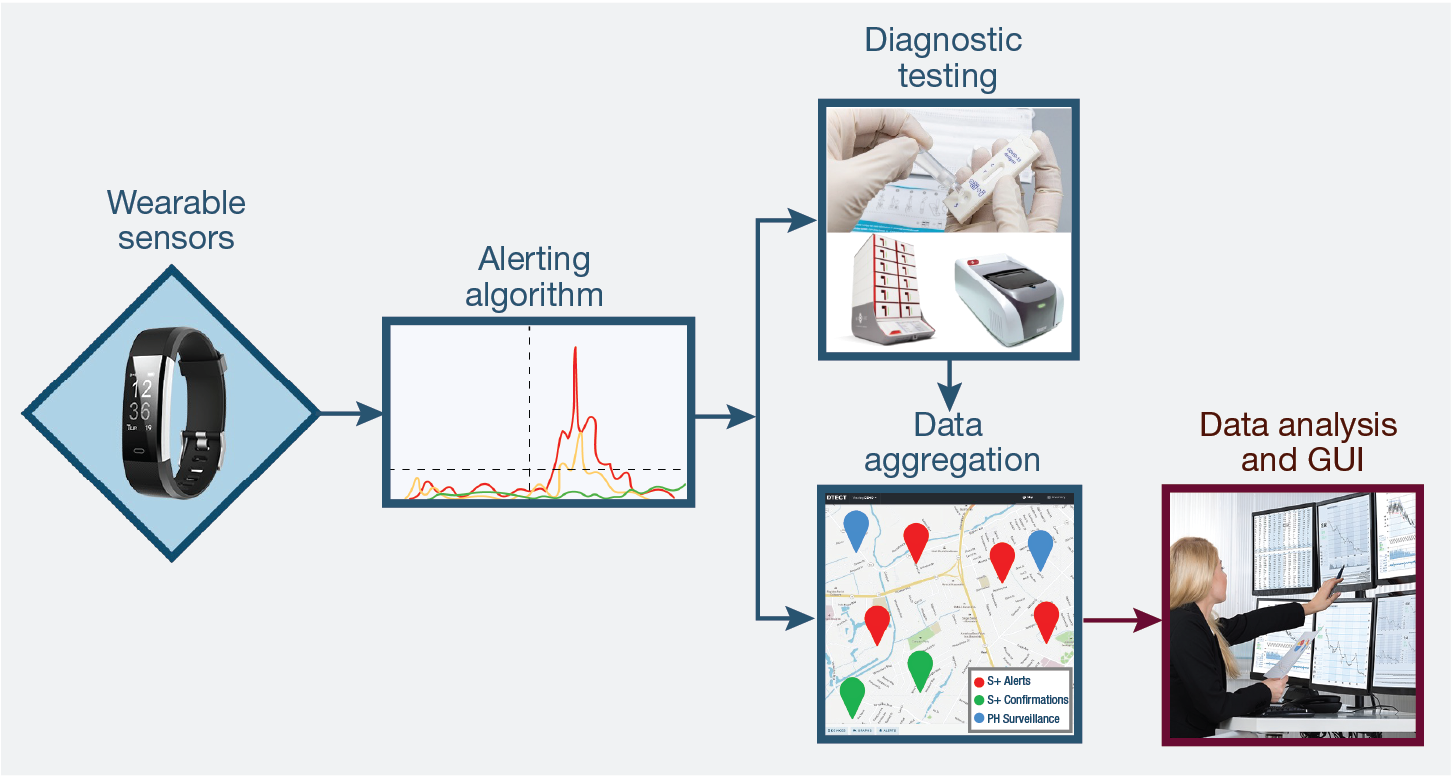
Figure 3
The wearable sensing and alerting architecture. Diagram of (a) the HSN subsystem, for collection, transmission, aggregation, and display of wearable data, and (b) its prototypical components for data collection (a commercial off-the-shelf fitness watch), data transmission (Bluetooth) to an auxiliary device (smartphone), local data analysis and transmission to HSN GovCloud for processing health risk scores and pushing alerts, and visualization (using Two Six Technologies’ proprietary “DTECT” platform). (Figure courtesy of RTI International)
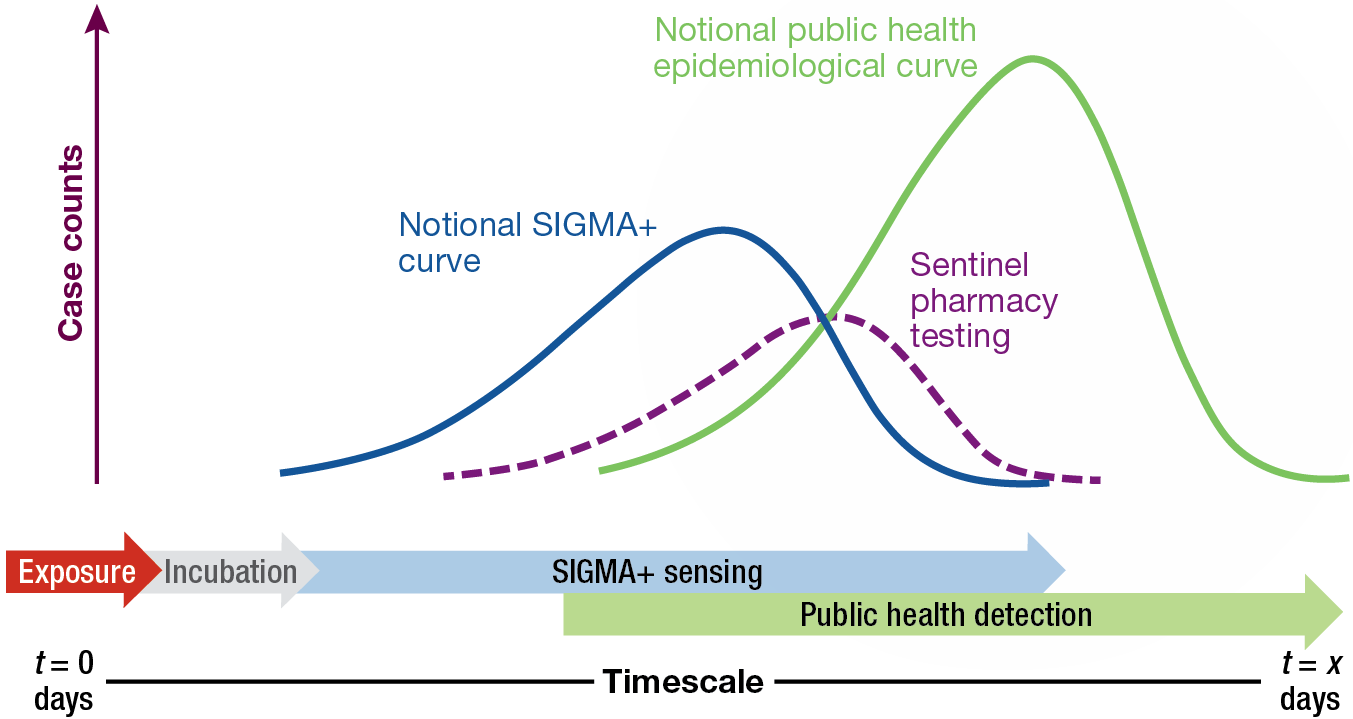
The strength of the HSN concept is its ability to monitor the health of a population and push real-time alerts to relevant stakeholders. In aggregate, these alerts could serve as early warning mechanisms, prompting a more expedient response than is traditional and subsequently mitigating the impact of the emergency (Figure 4). Further, the detection of pre- and asymptomatic illness provides critical data on the magnitude of the event that would otherwise be missed because some individuals never seek medical care and others may not know they have been impacted.
Figure 4
Figure 4. Notional epidemiological curves of disease incidence. Shown are incidence curves captured by means of traditional public health surveillance (green) and the two-tier HSN composed of wearable presymptomatic alerting (blue curve; tier 1), followed by presumptive identification through sentinel pharmacy testing (purple curve; tier 2).
HSN Use Case
The following is a use case for the HSN functioning as the sole SIGMA+ adjunct to public health entities.
Within a period of a few weeks in early summer, public health entities monitoring the HSN in a major US city notice an unseasonable and significant increase in wearable sensor-based alerts for respiratory illness. Local providers and hospitals are not yet reporting increases in visits or hospitalizations for respiratory illness, and syndromic surveillance is not indicating increases in over-the-counter cold and flu medication. Alerts begin to show clustering in more densely populated neighborhoods.
Public health entities issue an alert to local providers and hospitals to be vigilant for respiratory illnesses and to test suspected cases for viruses such as influenza and respiratory syncytial virus (RSV). People receiving alerts begin reporting to providers for evaluation and testing, and testing is negative for common respiratory pathogens. Isolate samples are sent to state public health laboratories for testing, and results are inconclusive. Isolates are sent to the Centers for Disease Control and Prevention, and public health entities begin case investigation interviews with affected persons to determine potential exposures and timelines, monitor symptoms, and characterize interaction networks.
Deployment of an HSN affords the following benefits:
- Even without positive diagnoses, the HSN can provide early warning of unusual disease activity to public health entities, permitting prompt and proactive investigation (including coordination with local care providers and hospital systems). This, in turn, enables earlier and more accurate determination of the seriousness of the situation.
- Temporal and geographic data in combination with testing results may be modeled to estimate asymptomatic infection rates, attack rates, and areas at high risk of spread. These data can help refine assessments of the outbreak’s significance. Further, these data can be used for more targeted epidemiological investigations, interventions, and testing strategies and to inform the use of nonpharmaceutical interventions such as wearing masks and limiting social gatherings.
- Enabling officials to investigate, mobilize resources, and intervene more quickly will reduce the spread of the virus and subsequently decrease morbidity and mortality associated with infection.
- During the early stages of the COVID-19 pandemic, after the virus was circulating in the United States, but before positive case identifications had begun in most cities, an HSN could have provided early indications of spread in specific regions, nuanced understanding of asymptomatic rates and disease severity, and information about transmission characteristics. This information could have supported government responses to the public health emergency and helped mitigate the impact of COVID-19.
HSN Stakeholder Landscape
Stakeholders in a notional HSN fall into three categories: participants, data providers, and end users. Participants include individuals outfitted with wearable sensors that actively transmit data to the HSN. This group may include members of the general public, first responders, and medical personnel. Data providers are nonparticipant entities that provide relevant contextual and surveillance-related data to the HSN. These entities may include hospitals, laboratories, syndromic surveillance networks, and environmental sensors. End users include those individuals who actively monitor and leverage data and analyses generated by the HSN to make decisions in the interest of public health. End users may include people in various levels of government public health, first responders, and members of law enforcement.
Nonmateriel Considerations
Several nonmateriel factors must be considered and addressed to ensure successful HSN system design and operational deployment. These factors include participant considerations, regulations, and data protection and management.
Adequate system performance relies on a sufficient number of participating adults in the population. Approaches to achieve the required participation threshold may include government support through device donations, subsidies, or incentivization; private or philanthropic organizations, insurance providers, or wearable sensor manufacture support; and citizen science or “bring-your-own-device” participation models. Further, factors such as lifestyle, privacy beliefs, or unfamiliarity with or distrust of commercial technology may preclude certain individuals from willingly participating.
The enabling technology of the HSN is the wearable physiological sensor, which can monitor physiological attributes, track location, and communicate the collected data about the wearer. Wearable sensors may be subject to compliance with a variety of regulations (e.g., the Health Insurance Portability and Accountability Act, or HIPAA). Thorough analysis of each regulation and collaboration with relevant agencies will be required.
The protection of personal information must be the highest priority. Transparent disclosure of the types of data, how they are used, and methods for safeguarding data must be clearly communicated to would-be participants. Safeguards at the highest level of government standards must be in place to protect against inadvertent or intentional release or access. The minimum amount of data must be collected to meet system performance thresholds, and data must be anonymized as much as possible.
Feedback on the CONOPS
A significant contributor to CONOPS development was feedback solicited during focus groups and TTXs. During these events, the infrastructure and functionality of the HSN were presented, followed by targeted questions and open discussion. Feedback on the HSN fell into two categories, capability and implementation and utilization, and is summarized below.
HSN Capability
- A wearable-based, two-tier HSN is conceptually well received and would add value to emergency and public health response.
- To be effective, high-fidelity data, such as GPS tracking/back-tracking and display of the triggering physiological parameters, should be displayed for cases requiring investigation.
- When possible, data should be integrated with biosensor, agent-specific data to support response.
- The HSN provides data and situational awareness, demonstrating more utility to support broader public health response than first responders.
HSN Implementation and Utilization
- Trust in the system is critical and may be low initially while it is unproven to individual users.
- Context is important: data from disparate sources must be aggregated and presented together to provide comprehensive situational awareness.
- Jurisdictional responsibility for data monitoring and action must be determined in advance.
Summary and Implementation Considerations
Based on computational modeling and analysis, stakeholder engagements, pilot HSN studies, and CONOPS/concept of employment analysis, an HSN network is both technologically and practically feasible and would provide value to public health authorities and other decision-makers, the emergency response community, and individual participants in the network. Wearable sensors with the required features, alerting algorithms, communications networks, analysis infrastructure (including algorithms), and user interfaces are all either demonstrated or achievable with current technology. Resolution of nonmateriel concerns, including meeting regulatory requirements, is likewise viable. Any implementation of an HSN will require close collaboration with stakeholders and end users to account for locally specific factors and will require cross-agency partnerships and development of a business model ensuring sufficient public participation.
Continued development of the HSN capabilities will require interfacing with existing public health systems to test and ultimately verify, through well-defined metrics, the HSN’s ability to enhance disease surveillance. Thus, a transition partner (or partners) will likely need to conduct advanced development activities, evaluate the HSN capabilities as part of an initial operational test, conduct a pilot study of the proposed technology, and address and document full-system life-cycle challenges before deployment.
An HSN pushes the boundaries of traditional biosurveillance by providing real-time early warning updates to public health and law enforcement professionals. Information provided by the HSN will provide targeted and expedient situational awareness and subsequent decision support to mitigate the impacts of the emergency in question.
Acknowledgments: The authors acknowledge valuable contributions from the following APL colleagues: Rebecca Eager, Ariel Greenberg, James Howard, Alison O’Hare, Alex Proescher, Christina Pikas, Travis Lim, and Joseph Warfield. This article leverages insights of the following SIGMA+ collaborators: Ann Hammer and Alexis Joiner of Sandia National Laboratories; Dorota Temple and David Dausch of RTI International; Kajal Claypool and Kevin Tangen of Massachusetts Institute of Technology Lincoln Laboratory; and John Magnus and John Hungerford of Two Six Technologies. This material is based on work supported by the Defense Advanced Research Projects Agency (DARPA) under Contract No. HR0011-22-D-0001. The views, opinions, and/or findings expressed are those of the author(s) and should not be interpreted as representing the official views or policies of the Department of Defense or the US government. Distribution Statement A: Approved for public release, distribution is unlimited.
- DARPA, “Broad Agency Announcement: SIGMA+ Sensors,” DARPA/DSO, HR001118S0035, Apr. 5, 2018.
- D. S. Temple, M. Hegarty-Craver, R. D. Furberg, E. A. Preble, E. Bergstrom, et al., “Wearable sensor-based detection of influenza in presymptomatic and asymptomatic individuals,” J. Infect. Dis., vol. 227, no. 7, pp. 864–872, 2023, https://doi.org/10.1093/infdis/jiac262.
- CDC, “Flu Season,” https://www.cdc.gov/flu/about/season/ (last reviewed Sep. 20, 2022).
- CDC, “U.S. Influenza Surveillance: Purpose and Methods,” https://www.cdc.gov/flu/weekly/overview.htm (last reviewed Oct. 13, 2023).
- C. L. Gibbons, M. J. J. Mangen, D. Plass, A. H. Havelaar, R. J. Brooke, et al., “Measuring underreporting and under-ascertainment in infectious disease datasets: A comparison of methods,” BMC Public Health, vol. 14, no. 1, pp. 1–17, 2014, https://doi.org/10.1186/1471-2458-14-147.
- C. M. Zipfel, V. Colizza, and S. Bansal, “Health inequities in influenza transmission and surveillance,” PLOS Computat. Biol., vol. 17, no. 3, art. e1008642, 2021, https://doi.org/10.1371/journal.pcbi.1008642.
- CDC National Syndromic Surveillance Program (NSSP), “What Is Syndromic Surveillance?” https://www.cdc.gov/nssp/overview.html (last reviewed Sep. 20, 2023).
Ivan Stanish is a project manager in APL’s Asymmetric Operations Sector. He has a B.S. in chemical engineering with a bioengineering option and a Ph.D. in chemical engineering with a minor in inorganic chemistry, both from the University of California, Los Angeles. He has 24+ years of technical, project/program management, and systems engineering experience that encompasses research, development, and acquisition efforts focused on the detection and defeat of chemical, biological, radiological, nuclear, and explosive threats. He has coauthored 15 publications, has contributed to multiple scientific conference proceedings, and holds two patents.
Jane E. Valentine is a data scientist, biomedical engineer, and project manager in APL’s Asymmetric Operations Sector. She has a B.S. in mathematics and French and a Ph.D. in biomedical engineering, both from Carnegie Mellon University. Her work focuses on using data to understand complex situations and processes and to support better decision-making. Notable projects include epidemiological and disease surveillance modeling and analysis, machine learning on health data, quantitative metrics (and associated dashboards) development for complex systems and processes, and decision support tool development.
Damon C. Duquaine is a public health epidemiologist, project manager, and supervisor in APL’s Asymmetric Operations Sector. He has a B.S. in biology and an M.P.H., both from the University of Michigan. His work focuses on population health, infectious disease, data analytics, hospital quality improvement, modeling and simulation, and patient safety experience.
Robert A. Stoll is a project manager in APL’s Asymmetric Operations Sector. He has a B.S. in mathematics and physics from Millersville University, an M.B.A. from Johns Hopkins University, an M.S. in optics from the University of Rochester, and a Ph.D. in engineering management from George Washington University. He has diverse technical and managerial expertise in systems engineering, program and project management, staff development, mathematical modeling, test and evaluation, and chem-biodefense.
Ray H. Mariner is an assistant program manager in APL’s Asymmetric Operations Sector. He has a B.S. in chemistry from Loyola College (now Loyola University Maryland) and an M.S. in homeland security management from the University of Maryland University College (now the University of Maryland Global Campus). He has 25+ years of experience as an analytical chemist and data scientist, with areas of expertise including analytical chemistry, data science, semantic modeling, threat modeling, and threat prioritization.
Dorsey R. Woodson is a program manager in APL’s Asymmetric Operations Sector. He has a B.A. in psychology from Syracuse University and an M.A. in human resources management from Webster University. He manages programs focused on technology development for counter–weapons of mass destruction situational awareness, with an emphasis on chemical, biological, radiological, and nuclear threats and related detection and defeat technologies. In this role, he directs the development and delivery of knowledge advantage and decision aid architectures, analytics, and tools.